Suicidal Ideation, Self-Injurious Behavior, and Suicidal Threats
Discretion is advised due to the heavy topics addressed below that may not be appropriate for everyone.
Check out the website and YouTube channel for more in depth information on borderline personality disorder criteria.
Borderline personality disorder is the only personality disorder that has suicidal behaviors/self-harm listed as a criterion, but it’s not necessarily the personality disorder that is at the highest risk for these behaviors. Because of the intense emotional pain experienced by those with borderline personality disorder, self-injurious behaviors are commonly why those with this condition seek help. Unfortunately, this contributes to some of the stigma associated with borderline personality disorder. So let’s unpack this heavy topic and discuss the DSM criteria of suicidal ideation, behavior, threats, and self-harm. We’ll uncover what self-harm looks like, why individuals with borderline personality disorder self-harm, the stigma about these behaviors, and what loved ones can do.
The DSM-5-TR Criterion
| Note: Text in these boxes are the exact words from DSM-5-TR1 |
|---|
| 5. “Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior1.” (p. 752) |
|---|
The fifth criterion under borderline personality disorder addresses suicidality and self-injurious behaviors, which are often why those with borderline personality disorder seek help. The “Diagnostic Features” section in the DSM-5-TR’s borderline personality disorder also notes that self-mutilation is very common, and might even happen during times of dissociation, because it can bring relief by atoning for being “bad” (self-punishment) or by helping the person understand they’re alive and can feel something. The “Associated Features” section in the DSM-5-TR’s borderline personality disorder discloses that while death by suicide can occur, especially when borderline personality disorder is paired with depressive disorders or substance disorders, “deaths from other causes, such as accidents or illness, are more than twice as common as deaths by suicide in individuals with borderline personality disorder (Temes et al. 2019).” There is also risk for permanent harm like physical handicaps due to self-mutilation or impulsive, risky behavior.
Remember: This ONE criterion is not sufficient for a diagnosis of borderline personality disorder. While it’s the only personality disorder with suicidal behaviors listed as a criterion, it’s not the only one with correlations for risk for suicide. Suicidal behaviors come up in other diagnoses. Also, not every individual with a diagnosis of borderline personality disorder engages in self-injurious behavior.
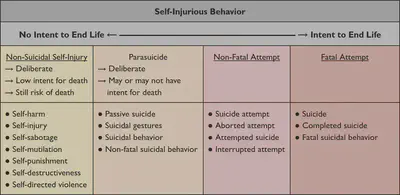
The Spectrum of Self-Injurious Behavior
The whole continuum of self-injurious behaviors are an outward expression of inward pain - a way to have pain seen. It can include physical behaviors, such as cutting, burning, choking, head banging, and punching. It can also include risky or reckless behaviors with intent to harm, including unsafe sexual encounters, risky meetups, substance abuse, reckless driving (i.e. driving too fast, intoxicated, unsafely), binge eating, restrictive eating, or excessive exercise.
Triggers and Causes
Because of the intense emotional pain experienced by those with borderline personality disorder, major stressors and/or changes can lead to self-injurious behavior. Losses and separations like job loss, divorce, and difficulties in school - basically when facing a threat of abandonment or rejection - can commonly lead to hopelessness and thus self-injurious behavior. Additionally, facing increased responsibility can lead to intense pain because there’s a threat to their dependence, and dependence ensures they stay connected to someone. They might feel like they can’t do something on their own and need to be taken care of; therefore, if they don’t have someone to care for them, they’ll feel alone, which is intolerable. This can make it seem like and feel like the motivation behind the self-injurious behavior is consciously manipulative (it can be in rare cases), but more than anything it’s an outward expression of an inner self-loathing: an external extension of internal pain.
Motivations & Stigma
There’s some pretty intense stigma around self-harm in those with borderline personality disorder that their self-harm is only manipulative or only for attention. I think this stigma stems from a help-seeking/help-rejecting dynamic in which those harming themselves can unconsciously do so to punish themselves but also to punish the person who “failed” to help them. It’s anger turned toward the self, and it’s often quite impulsive and reflexive. (Remember borderline personality impulsivity damages the self, while antisocial personality impulsivity damages the world). The primary motivation underlying self-injurious behavior in those with borderline personality disorder is a cry for help. It’s an unspoken, “See my pain. I can’t be alone. Save me.” Now there is also a secondary motivation that consists of distraction from pain.
Purpose
So what is the purpose of self-injurious behavior? It serves as a solution to decrease pain, like a coping mechanism. It’s a cry for help. It can help relieve internal pain or negative emotions, transferring the inner pain to physical pain. It results in eliciting responses from the environment that are reinforcing and soothing (i.e. utilizing beta endorphins, dopamine, serotonin), or even addictive. It can help someone feel alive, like they exist, grounding them in their physical self, though it could also increase numbness and dissociation. It can serve as a sense of control, to punish the self, to express self-hatred, or to express anger at others. All of these are based in deep and intense inner pain.
What Can Loved Ones Do?
It’s super scary to know someone you love is hurting themselves, and it might make you feel helpless or even guilty. So what do you do? Understand you don’t have to be alone in this. Seek professional help! You can also encourage your loved one to seek treatment, but you can’t make them go. You’re not responsible if they don’t go to treatment. Take care of yourself and your needs. Take responsibility for your own behavior but also keep yourself in reality. Don’t get sucked into the pull to take their actions personally. Increase your awareness of any behaviors you’re engaging in that are reinforcing or enabling their self-injurious behavior. Gently and clearly, without defensiveness, communicate, set, and keep boundaries.
Sometimes safety planning is needed, especially if there are episodes of rage (both toward self and others). Keep boundaries! If necessary, leave to a designated safe space or call the authorities. Remember:
- Don’t ignore the person. You can say, “I will talk with you when you’re calm.”
- Don’t respond with your own rage. Stay calm.
- Don’t hurt the other person. Refrain from fueling the fire.
- Don’t take responsibility for their actions!
While the spectrum of self-injurious behavior may or may not show up in someone diagnosed with borderline personality disorder, it’s notable enough to be its own criterion in the DSM-5-TR. There’s a lot of stigma associated with it, and it spans a whole continuum. It can be triggered by many different things and motivated by pain. It can feel manipulative, but most times that’s not the intent. Regardless, remember to seek professional help and maintain boundaries! It’s easier said than done, but see below for some helpful resources. You’re not alone.
RESOURCES
Crisis and Suicidal Ideation
- Crisis Link
- Crisis Text Line (Text HOME to 741-741)
- National Hopeline Network
- National Suicide Prevention Lifeline - 988
- American Foundation for Suicide Prevention
Mental Health Resources with Multiple Domains
- Black Emotional and Mental Health Collective
- The Mental Health Coalition - Crisis Resources
- The JED Foundation
- SAMHSA 988 Toolkit
- National Alliance on Mental Illness (NAMI) - Support Groups
Additional References
- https://www.nationalelfservice.net/mental-health/self-harm/self-harm-terminology/
- https://en.wikipedia.org/wiki/Self-harm#Classification_and_terminology
- Temes, C. M., Frankenburg, F. R., Fitzmaurice, G. M., & Zanarini M. C. (2019). Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. Journal of Clinical Psychiatry, 80(1). https://doi.org/10.4088/JCP.18m12436
-
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders: DSM-5-TR (5th edition, text revision.). https://doi.org/10.1176/appi.books.9780890425787 ↩︎ ↩︎






